Being Good!
Introduction
Most of us at one time in our lives have been asked by someone to be good. So what does “good” mean? The Oxford dictionary defines “good” in many ways. As an adjective to be “good” is to be desired or approved, having the required qualities; of a high standard, possessing or displaying moral virtue, giving pleasure; enjoying or satisfying, thorough, valid.
This diversity in its definition has extended the use of the word “good” to describe institutions, processes and outcomes such as good hospitals, good practice, good governance and good health.
Good Characters
Good governance needs good people among them good doctors. However, defining a good doctor is not a simple issue and depends through which perspective it is attempted. Healthcare professionals such as doctors, nurses, pharmacists, etc may see goodness in different ways and their view may be different again from how patients view goodness.
The Health Governance Unit attempted to define the good doctor and elaborate on the differences in its definition through an open ended question that was directed to a group of peers and a group of inpatients asking them about the characteristics that they thought would make a good doctor.
The top ten characteristics of a good doctor as mentioned by peers (see below left) were: knowledgeable, respectful, communicator, professional, updated, honest, empathetic, evidence-based, listener, and being patient.

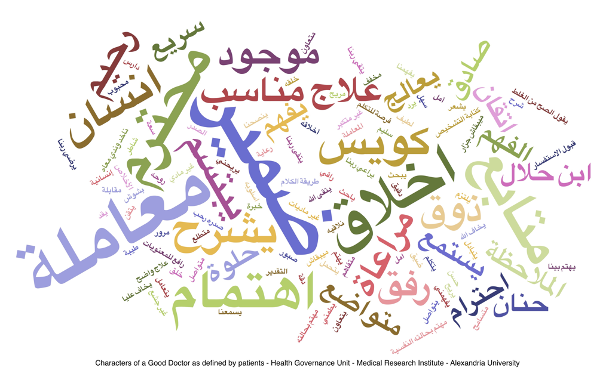
The top ten characteristics of a good doctor as mentioned by patients in their own words in Arabic (see below right) were: ضمير and معاملة and أخلاق and إهتمام and محترم and متابع and يتقى ربنا and إنسان and كويس and يشرح. See back for translation.
It is clear that peers and patients have different perspectives of what makes a good doctor. Peers see a good doctor as a person who is primarily competent in his work (speciality) supported by professional, ethical, human and interactive capabilities.
On the other hand, patients see a good doctor as one who is ethical, human and interactive in his or her behavior. This emphasis could also stem from what is currently lacking in the patient-doctor relationship.
Defining characteristics of a good doctor, especially within a local context, is important as it is the ideal guide for local educational curricula and local professional development programs content.
The Health Governance Unit presents the Good Doctor Framework (GDF) as a conceptual structure for human excellence in healthcare.
The GDF is based on the characters of a good doctor as seen by peers and patients. Similar characters have been grouped under five headings as shown in the figure opposite. The five domains are not mutually exclusive as some attributes could fit into several domains.
GDF could be used in many ways. It can be used as either a framework for assessment, continuing professional development, or as a framework for the development of undergraduate or postgraduate curricula.
GDF can also help individuals in their reflection on their progress and in ensuring a balance between the attributes of the framework. The framework is applicable to the various career stages an individual goes through, such as education, training and ultimately practice.
Good Doctor Framework
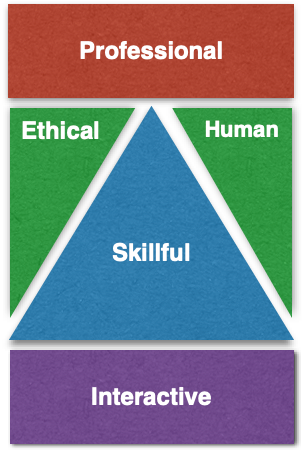
Skillful
Relating to the intellectual and hands-on clinical skills of the doctor including capacity to apply acquired knowledge, analyze patient symptoms and signs, synthesize a diagnosis and evaluate treatment outcome. A good doctor should also acquire practical skills related to clinical examination, diagnostic procedures and therapeutic interventions. A good doctor should ensure that his or her skills are updated and maintained.
Professional
Work related areas, away from hands-on-treatment, that impact doctor efficiency, including capacity to plan and make decisions based on a vision and situation analysis (information), risk aversion, practice review (audit), and reflection.
Interactive
Relating to the capacity of the doctor to influence others and being influenced by others, including communication, teamwork, patient and public engagement, collaboration, knowledge and experience sharing, mentoring.
Ethical
Behavior related to moral issues often unseen by the patient, such as confidentiality, respect, working for the good of patients, protecting the vulnerable, disclosure of research interests and relationships with industry including financial arrangements.
Human
Behavior related to perceived or actual relationship with patients and colleagues, especially characteristics that affect their emotional state such as empathy, sympathy, advocacy, listening, caring, supportive.